Surgical Procedures By Prof Kader
ACL
Professor Kader is specialised in knee sports surgery. Over the years he has looked after many professional and semi-professional athletes.
Most common procedures in the knee are
Knee Arthroscopy for meniscal excision or repair
Chondroplasty or Microfracture..etc
ACL reconstruction or Revision ACL reconstruction
PCL reconstruction
Multiligament reconstruction

Anterior cruciate ligament reconstruction
The anterior cruciate ligament (ACL) is 3cm long band of fibrous tissue that connects the femur (thigh bone) to the tibia (shin bone).
Its function is to resist and limit internal rotation and forward movement of the tibia. Damage to the ACL can cause the knee to give way, twist and pivot. This can be very painful and could cause damage to the rest of the joint such as the articular cartilage (bearing surface cover) and the menisci (semilunar soft cartilage). When both bundles are damaged this is called complete rupture however injury to one bundle is called partial rupture.
Anterior cruciate ligament reconstruction has become one of the most commonly performed surgical procedures to the injured knee joint. The rationale for surgical treatment is to stabilise the knee joint and prevent it from buckling under load. Joint stabilisation has been shown to decrease meniscal and articular cartilage damage which potentially decreases the incidence and severity of later osteoarthritic change. Therefore, patients are strongly advised to refrain from playing competitive sport prior to surgical reconstruction as this may lead to irreparable damage to the joint cartilage or menisci.
Surgical techniques have advanced greatly over the past decade along with post-operative management protocols. This, in part, has been driven by patient non-compliance with traditional protocols. Accelerated rehabilitation protocols have been developed and in this paper is defined as – immediate full weight bearing, immediate full extension and immediate active and passive mobilisation of the knee joint.
As surgical techniques have become more accurate and less invasive with the advent of arthroscopic techniques, post-operative morbidity has decreased.
Preparation and expectation
You should inform your surgeon and anaesthetist, of any medical conditions, allergies or previous medical treatment.
It is extremely important that there are no cuts, on your lower limb as this greatly increases the risk of infection. Please DO NOT shave or wax your legs for one week prior to surgery. The surgeon will shave around the knee just before the procedure.
Patients should stop smoking and taking oral contraceptive pill one week prior to surgery as this increases the risk of thrombo-embolism (life threatening blood clots). Smoking also causes wound infection and weaken the graft.
After the operation you will be required to stay in hospital for few hours. Overnight stay may be required due to the affects of the anaesthetic or an inability to manage crutches. Some patients prefer to stay overnight following their surgery if they are having significant pain or have a long distance to travel home.
Physiotherapy is commenced immediately post operatively. Your own physiotherapist will supervise muscle contractions, crutch walking and weight bearing. Physiotherapy should continue on a daily basis. The sutures are removed 7-10 days following surgery. By this time, you should be able to walk without crutches. Sedentary and office workers may return to work approximately 2-3 weeks following surgery. Most patients should be able to walk normally 14 days following surgery although there is considerable patient to patient variation.
Driving is permitted when you are able to walk without crutches.
Physiotherapy is continued intensively until 6 weeks when jogging under controlled conditions is commenced.
Football or any contact sport should be avoided for 9-12 months. A return to competitive sport is permitted at 9-12 months following surgery, provided that there has been a complete rehabilitation and the joint is demonstrated to be stable. Please do not play football any earlier as you risking graft rupture. The surgeon may allow earlier return to professional sport if he deems its appropriate.
Playing sport non-competitively or training is possible at 4 -6 months. Training may commence when an adequate rehabilitation of the thigh musculature has occurred.
The surgery
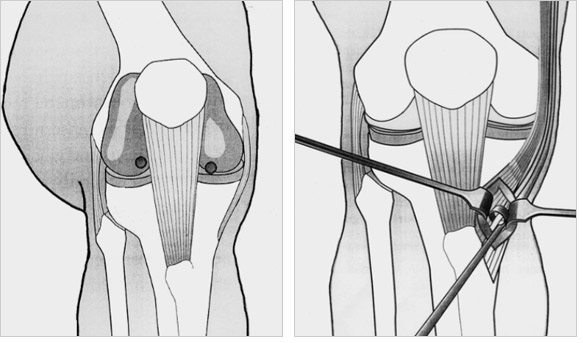
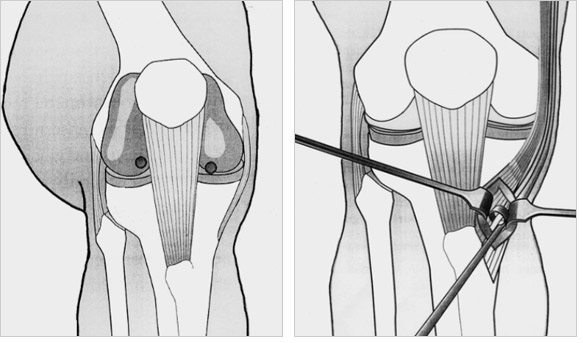
Arthroscopic surgery removes the ruptured anterior cruciate ligament stumps and any concomitant meniscal surgery is carried out. Articular cartilage damage and other pathology is then noted by the surgeon as these may affect the post-operative management protocol.
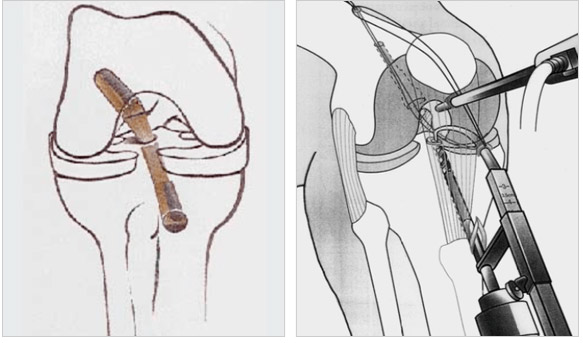
An autologus graft is harvested – mid-third patellar tendon or semitendinosus and gracilis tendon. This graft is then prepared and placed with the joint in an isometric and anatomic position. A graft so placed will allow a full range of joint motion without undue force on its fibres. Current fixation techniques include interference fit screw fixation, endobutton and suture and post fixation techniques. These have been shown, in experimental studies, to have enough immediate rigidity of fixation to allow an accelerated mobilisation programme. As many of these patients now have their surgical procedure carried out on an out-patient basis in a day surgery, the physiotherapy regime is frequently commenced the following day in the physiotherapy clinic.
Arthrofibrosis is more frequently seen in those patients who undergo acute anterior cruciate ligament reconstruction or have concomitant capsular and collateral ligament damage. Therefore, we recommend a period of joint cooling down before offering ligament reconstruction.
Postoperative problems
Postoperative bleeding & marrow exuding from the bony tunnel may track down the shin causing red inflamed painful areas. Characteristically when standing up the blood rushes to the inflamed area causing throbbing which should ease with elevation and ice packs. This may end with a bruise and slight swelling around the ankle usually lasting about 1 week. This is a normal postoperative reaction and only delays short term recovery. Wound bruising is very common so please don’t be alarmed by blue discoloration of the skin and don’t use antibiotics unnecessarily
Due to the skin incision patients may notice a numb patch on the outer aspect of their leg past the skin incision. This is of no functional significance and is unavoidable. The numb patch tends to shrink with the passage of time and does not affect the result of the reconstructed ligament.
Your hamstring musculature will recover quickly and tendon regrowth may be felt at 14 days following surgery. However, scar tissue forms around the reformed tendons. This frequently tears and is felt as a pop or tear behind the knee on the inner side. This will usually set your rehabilitation back a few days only. Scar tissue may tear more than once but does not usually occur following 6-8 weeks post operative.
Complications related to surgery
Deep vein thrombosis and pulmonary embolus:
Although this complication is rare following arthroscopic surgery, a combination of knee injury, prolonged transport and immobilisation of the limb, smoking and the oral contraceptive pill or hormonal replacement therapy all multiply to increase the risk. Any past history of thrombosis should be brought to the attention of the surgeon prior to your operation. The oral contraceptive pill, hormonal replacement therapy and smoking should cease one week prior to surgery.
Excessive bleeding resulting in a haematoma is known to occur with patients taking aspirin or nonsteroidal anti-inflammatory drugs.
Restricted range of motion, due to excessive scarring within the joint, or an inadequate mobilisation at physiotherapy may require arthroscopy to divide the adhesions or manipulation to overcome the adhesions. This will be assessed at 6 weeks post operative.
Graft failure due to poorly understood biologic reasons occurs in approximately 1% of grafts and a further 1% of grafts rupture during the rehabilitation programme.
Surgery is carried out under strict germ free conditions in an operating theatre. Antibiotics are administered intravenously at the time of your surgery. Any allergy to known antibiotics should be brought to the attention of your surgeon or Despite these measures, following arthroscopic ACL reconstructive surgery there is a less than 1 in 500 chance of developing an infection within the joint. This may require treatment with antibiotics or may require hospitalisation and arthroscopic draining of the joint with intravenous antibiotics. Subsequent to such procedures prolonged periods of antibiotics are required and the post operative recovery is slowed.
Please do not shave or wax your legs prior to surgery and report any skin abrasions or cuts to your surgeon.
Please do not touch the wounds after surgery unless your hands are cleaned
As with all operations if at any stage anything seems amiss it is better to call up for advice rather than wait and worry. A fever, or redness or swelling around the line of the wound, an unexplained increase in pain should all be brought to the attention of the surgeon and his team.
AIMS of physiotherapy
Physiotherapy should ideally commence pre-operatively. Patients who have a pain free, mobile, healthy joint recover far quicker and with less complication than those with surgery carried out on acutely painful joints. Even patients with chronic injuries benefit from pre-operative assessment and pre-operative “programming”. It has been our experience that if patients have learnt the exercises required pre-operatively they have fewer problems with these exercises post-operatively.
As stated earlier, many patients now have their procedure carried out as out-patients in a day surgery and their physiotherapy is commenced in the acute post-operative stage the same day.
Over the next three to six months the following are treatment goals.
Diminish post-operative pain and swelling.
Pain and swelling occurs from two areas,
First, the joint with post-operative effusion and quadriceps inhibition
Secondly, from the donor site be it patellar tendon or hamstring tendon.
Restore a full range of motion.
Restore muscle tone and strength.
Maintain and develop aerobic conditioning.
Proprioceptive retraining allowing a safe return to work and sport as soon as possible.
Rationale of programme designs
This programme has been based on the following known information regarding anterior cruciate ligament reconstructive surgery.
Early mobilisation has advantages such as maintenance of articular cartilage nutrition, retention of bone mineralisation and helps to prevent arthrofibrosis. Braces, if used, should be aimed at obtaining full extension. Progressive controlled loading of the graft provides a stimulus for collagen healing and regeneration. This is a needed stimulus for growth. It is very difficult to overload a graft placed in the correct isometric and anatomic position.
Weight bearing has not been shown to be detrimental to the graft and progression to full weight bearing is allowed as rapidly as pain permits.
It is assumed that the technical aspects of the surgical procedure allow for immediate graft fixation sufficient to allow aggressive mobilisation. This fixation to bone improves with the passage of time as the attachment “ligamentises”. It is also based on the assumption that the graft is probably never stronger than the day it is implanted.
Kinematic research has shown that open chain extension exercises cause significantly more anterior tibial displacement (and force on the graft) than closed chain activities.
With injury to the joint resulting in the loss of the anterior cruciate ligament’s function, there is also a significant loss to the joints mechanoreceptors. Therefore, a large emphasis must be placed on proprioceptive retraining prior to the return to unrestricted sporting activities.
The staged programme
Stage I Control Inflammation
Time Period: Day 1 to Day 10-14 (sutures removed)
AIM:
Post-operative pain relief and management of soft tissue surgical trauma.
Get the patient off crutches and walking normally.
Goals:
Wound healing.
Manage the graft donor site morbidity, i.e. pain and swelling.
Decrease joint swelling.
Restore full extension.
Establish muscle control.
Possible problems:
Infection – the patient complains of a constant, severe pain (throbbing with every heart beat). The patient is sweaty, ill and has a tense effusion. If no prophylactic antibiotics were given at surgery, infection usually occurs within the first 72 hours. However, if prophylactic antibiotics were given at surgery (as is usually the case), infection may come on insidiously 5-10 days post operatively.
Post operative haemorrhage into the graft donor site. This results in a red, hot, tender area. Joint motion is not usually restricted except when pressure is placed on the graft donor site. Characteristically the patient complaints of pain when blood rushes to the donor site upon standing or hanging the limp dependent.
Hamstring strain or pain. Deep venous thrombosis. The patient has calf, popliteal, thigh or groin pain and tenderness, with associated swelling of the limb. Stiffness due to early arthrofibrosis or reflex sympathetic dystrophy.
Treatment guidelines:
Reduction of swelling and pain using ice, elevation, co-contractions and pressure pump.
Partial weight bearing to full weight bearing as pain and swelling allows.
Active range of motion aiming for full extension by 14 days. Flexion will come without a great effort.
Patella mobilisations to maintain patella mobility.
Gait retraining with full extension at heel strike.
Due to post operative pain and swelling, early return of coordinated muscle function may be encouraged with the use of biofeedback and selective muscle stimulation if necessary. Caution should be taken following patellar tendon grafts in stimulating the quadriceps mechanism as patella fracture has been reported.
Early active quadriceps strengthening is begun as a static co-contraction with hamstrings emphasizing VMO control at various angles of knee flexion and progressed into weight bearing positions.
Gentle hamstring stretching is initiated immediately to minimise painful adhesions. Hamstring tears with the patient reporting a ‘pop’ about the posteromedial thigh is common within the first 14 days and even within the first 6 weeks.
Early active hamstring strengthening begins with static weight bearing co-contractions and progresses to active free hamstring contractions by day 14. Resisted hamstring strengthening should be avoided for at least 4-6 weeks.
At 10-14 days post operatively, the dressings will be removed and the wound checked.
NB: Quadriceps exercises are to be closed chain only during the first four stages.
StageII Hamstring and quadriceps control
Time Period: 2-6 weeks
AIM:
To return the patient to normal function.
Prepare the patient for Stage III.
Goals:
Obtain a full unrestricted range of motion.
Develop good muscle control and early proprioceptive skills.
If not done sooner, restore a normal gait.
Reduce any persistent effusion.
Possible complications:
Stiffness.
Recurrent hamstring strain.
Increasing laxity of the graft.
Graft failure.
Treatment guidelines:
Aim for a full range of motion using active and passive techniques.
Progress co-contractions for muscle control by increasing the repetitions, length of contraction and more dynamic positions, e.g. two leg quarter squats, lunges, stepping, elastic cords.
Commence swimming once the wound has healed.
Gym equipment can be introduced gradually such as stationary bike, stepper, leg press, mini trampoline.
If swelling is persistent, continue with the use of a pressure pump, ice and static quadriceps exercises. Hold back on gym activities until the effusion is settling.
Hamstring strengthening automatically progresses with the increased complexity and repetitions of co-contractions. Open chain hamstring exercises are also included at this stage although often they are painful. It is important to concentrate on hamstring stretches and to incorporate resistance gradually to prevent recurrent injury.
Weeks 3-4:
Low resistant (e.g. 1-2Kg ankle weight) bilateral hamstring curls are progressed to low resistant unilateral curls as pain allows.
Weeks 4-6:
Care must be taken as hamstring straining may occur and impede further progression. Low resistance, high repetition weights aim to increase hamstring muscle endurance. Continue with intensive stretching exercises.
Week 6:
Eccentric hamstring strengthening is progressed as pain allows. Hamstring curl equipment can be introduced.
Consider beyond the knee joint for any deficits, e.g. gluteal control, tight hamstrings, ITB, gastric and soleus, etc.
NB: With the accelerated programme patients can feel very confident by 6 weeks. However, it must be stressed that the graft is still not mature and they must be aware of their functional restrictions to avoid the risk of graft failure.
Stage III Proprioception
Time Period: 6-12 weeks
AIM:
Improve neuromuscular control and proprioception.
Goals:
Continue to improve total leg strength.
Improve endurance capacity of muscles.
Improve patient confidence.
Possible problems:
Arthrofibrosis
Patello-femoral irritability.
Chronic inflammation.
Graft laxity and rupture.
Treatment guidelines:
Progress co-contractions to more dynamic movements, e.g. step lunges, half squats.
Proprioceptive work should be more dynamic, e.g. lateral stepping, slide board etc.
Can begin jogging in straight lines on the flat.
Progress resistance on gym equipment such as leg press and hamstring curls. Hamstring strengthening programme aims for a progression in both power and speed of contraction.
Start cycling on normal bicycle.
Continue with static control but emphasize endurance, e.g. wall squats.
Consider pelvic and ankle control plus cardiovascular fitness.
NB: Still no open chain quadriceps exercises. Solo sports such as cycling, jogging and swimming are usually permitted with little or no restrictions during this stage.
StageIV Sport specific
Time Period: 12 weeks to 5 months
AIM:
Prepare to return to sport.
GOALS:
Incorporate more sport specific activities.
Introduce agility and reaction time into proprioceptive work.
Increase total leg strength.
Develop patient confidence.
Possible problems:
Patello-femoral irritability.
Treatment guidelines:
Progressing of general strength work, e.g. half squats with resistance, leg press, leg curls, wall squats, step work on progressively higher steps, stepper and rowing machine.
Proprioceptive work should include hopping and jumping activities and emphasis a good landing technique. Incorporate lateral movements.
Agility work may include shuttle runs, ball skills, sideways running, skipping rope, etc.
Low impact and step aerobics classes help with proprioception and confidence.
Pool work can include using flippers.
Sport specific activities will vary for the individual, e.g. Tennis – lateral step lunges, forward and backwards running drills: Skiing – slide board, lateral box stepping and jumping, zigzag hopping; Volleyball or Basketball – vertical jumps.
NB: The above activities are gradually introduced throughout Stage IV.
Stage V Return to sport
Time Period: 7-8 months or longer
Goals: Return to sport safely and with confidence.
Treatment guidelines:
Can Safely do open chain quadriceps work, (i.e. leg extensions).
Continue progression of plyometric and sport specific drills.
Return to training and participating in skill exercises.
Continue to improve power and endurance.
Advice may be needed as to the need for modifications to be able to return to sport, e.g. Football – start back training in running shoes or short sprigs. Will usually return to lower grades initially; Skiing – stay on groomed slopes and avoid moguls and off piste initially. Racers may initially lower their DIN setting on the bindings.
Appendix
Co-Contraction Exercises
In relation to the knee these exercises ensure that both the hamstring muscle group and the quadriceps muscle group contract simultaneously to achieve a bracing effect on the knee joint.
Not only will these two groups be contracting, however, but stabilisers above and below will also contract such as gluteals, psoas, TFL, adductors and calf muscles.
To initially teach a co-contraction, it is easiest to place a rolled pillow under the knee and ask the patient to push into the pillow. This will switch on the hamstrings and gluteals. They should then tighten the quadriceps.
A co-contraction should initially be held for approximately 15 seconds.
Open -v- Closed Chain Exercises
Closed kinetic chain exercises are performed with the foot placed on a surface (e.g. floor, step, pedal) and the entire limb is bearing an axial load.
Joint compression occurs when the limb is loaded by body weight and this provides inherent joint stability and allows more strenuous strengthening without the degree of shearing forces, or anterior tibial displacement that occurs with conventional open kinetic chain exercises. Closed chain exercises performed with co-contraction of hamstrings and quadriceps also lessen the patello-femoral joint surfaces.
The closed exercises place functional stresses on the joint and entire limb. These exercises can easily be designed to be specific to normal weight bearing activities used for ACL as well as sport.
Plyometrics
Plyometrics exercises are characterised by very powerful muscle contractions in response to a dynamic loading or stretching of the muscles involved in the exercise. The muscles are pre-loaded with an eccentric contraction before a powerful concentric contraction.
Plyometrics help to improve muscle power in the later stage of rehabilitation. Examples are box drop jumps, bounding and hopping.
Information sheet for patients who have ruptured
their anterior cruciate ligament
Sports Injury Clinic www.deiarykader.co.uk Professor Deiary Kader
The anterior cruciate ligament (ACL) is a 38mm long band of fibrous tissue that connects the femur (thigh bone) to the tibia (shin bone). Its function is to control and limit the amount of forward movement of the outer side of the joint when performing twisting actions.
Surgical Treatment
Patients who are unable (generally young adults) or those unwilling to lower their level of activity, are at risk of causing further damage to their knee should they return to sporting activity and are advised to undergo surgical reconstruction.
Patients are strongly advised to refrain from playing competitive sport prior to surgical reconstruction as this may lead to irreparable damage to the joint cartilage or menisci.
All reconstructive procedures for the ACL require a graft. Our reconstructive technique involves grafting the torn ACL with segments of your hamstring tendons. This technique utilises specially designed screws allowing secure immediate fixation of the tendon within the joint allowing for a rapid rehabilitation, dispensing the need for a brace or plaster. The surgery is frequently carried out as a day surgery procedure. A 95% success rate is normal with some deterioration over time depending upon other damage within the joint. Our long term results suggest that stabilising the joint protects menisci and thus lessening later osteoarthritic degenerative change. Although ACL reconstruction surgery has a high probability of returning the knee joint to near normal stability and function, the end result for the patient depends largely upon
1- Satisfactory rehabilitation
2- The presence of other damage
Graft Harvest:
Through a single incision the hamstring tendons are removed
to be used for the graft.
Tunnel Drilling:
Small tunnels are drilled in the bone to prepare for
graft fixation.
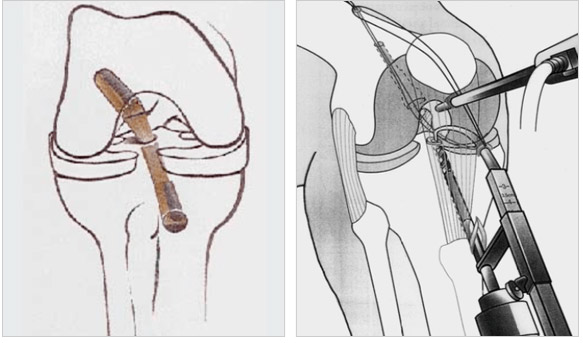
Arthroscopy: Using an arthroscope through the two small incisions the surgeon will remove the torn ACL and perform required meniscal surgery.
Graft Fixation: The graft is inserted into the drilled tunnels and fixed in place with screws. Depending on bone quality, supplementary fixation, in the form of a staple may also be required.
What is involved for the patient

- You should inform your surgeon and anaesthetist, of any medical conditions, allegries or previous medical treatment.
- It is extremely important that there are no cuts, on your lower limb as this greatly increases the risk of infection. Please DO NOT shave or wax your legs for one week prior to surgery.
- Patients should stop smoking and taking oral contraceptive pill one week prior to surgery as this increases the risk of thrombo-embolism (life threatening blood clots). Smoking also causes wound infection and weaken the graft.
- After the operation you will be required to stay in hospital for few hours. Overnight stay may be required due to the affects of the anaesthetic or an inability to manage crutches. Some patients prefer to stay overnight following their surgery if they are having significant pain or have a long distance to travel home.
- Physiotherapy is commenced immediately post operatively. Your own physiotherapist will supervise muscle contractions, crutch walking and weight bearing. Physiotherapy should continue on a daily basis. The sutures are removed 7-10 days following surgery. By this time you should be able to walk without crutches. Sedentary and office workers may return to work approximately 2-3 weeks following surgery. Most patients should be able to walk normally 14 days following surgery although there is considerable patient to patient variation.
- Driving is permitted when you are able to walk without crutches.
- Physiotherapy is continued intensively until 46 weeks when jogging under controlled conditions is commenced.
- Football or any contact sport should be avoided for 9-12 months. A return to competitive sport is permitted at 9-12 months following surgery, provided that there has been a complete rehabilitation and the joint is demonstrated to be stable. Please do not play football any earlier as you risking graft rupture.
- Playing sport non-competitively or training is possible at 4-6 months. Training may commence when an adequate rehabilitation of the thigh musculature has occurred.
Minor Effects of Surgery.
- Postoperative bleeding & marrow exuding
from the bony tunnel may track down the shin causing red inflamed painful areas. Characteristically when standing up the blood rushes to the inflamed area causing throbbing which should ease with elevation and ice packs. This may end with a bruise and slight swelling around the ankle usually lasting about 1 week. This is a normal postoperative reaction and only delays short term recovery. Wound brusing is very common so please don't be alarmed by blue discolartion of the skin and don't use antibiotics unnecessarly
- Due to the skin incision patients may notice a numb patch on the outer aspect of their leg past the skin incision. This is of no functional significance and is unavoidable. The numb patch tends to shrink with the passage of time and does not affect the result of the reconstructed ligament.
- Your hamstring musculature will recover quickly and tendon regrowth may be felt at 14 days following surgery. However scar tissue forms around the reformed tendons. This frequently tears and is felt as a pop or tear behind the knee on the inner side. This will usually set your rehabilitation back a few days only. Scar tissue may tear more than once but does not usually occur following 6-8 weeks post operative.
Complications related to surgery
- Deep vein thrombosis and pulmonary embolus: Although this complication is rare following arthroscopic surgery, a combination of knee injury, prolonged transport and immobilisation of the limb, smoking and the oral contraceptive pill or hormonal replacement therapy all multiply to increase the risk. Any past history of thrombosis should be brought to the attention of the surgeon prior to your operation. The oral contraceptive pill, hormonal replacement therapy and smoking should cease one week prior to surgery.
- Excessiv
e bleeding resulting in a haematoma is known to occur with patients taking aspirin or nonsteroidal anti-inflammatory drugs.
- Restricted range of motion, due to excessive scarring within the joint, or an inadequate mobilisation at physiotherapy may require arthroscopy to divide the adhesions or manipulation to overcome the adhesions. This will be assessed at 6 weeks post operative
- Graft failure due to poorly understood biologic reasons occurs in approximately 1% of grafts and a further 1% of grafts rupture during the rehabilitation programme.
- Surgery is carried out under strict germ free conditions in an operating theatre. Antibiotics are administered intravenously at the time of your surgery. Any allergy to known antibiotics should be brought to the attention of your surgeon or anaesthetist. Despite these measures, following arthroscopic ACL reconstructive surgery there is a less than 1 in 400 chance of developing an infection within the joint. This may require treatment with antibiotics or may require hospitalisation and arthroscopic draining of the joint with intravenous antibiotics. Subsequent to such procedures prolonged periods of antibiotics are required and the post operative recovery is slowed
Please do not shave or wax your legs prior to surgery and report any skin abrasions or cuts to your surgeon.
Please do not touch the wounds after surgery unless your hands are cleaned
As with all operations if at any stage anything seems amiss it is better to call up for advice rather than wait and worry. A fever, or redness or swelling around the line of the wound, an unexplained increase in pain should brought to the attention of the surgeon. Please Call prof Kader's team
Antro lateral Ligament (ALL)
Can rupture with the ACL creating a very unstable knee. This is a photograph of the lateral side of the knee showing the lateral collateral ligament (LCL) and the antrolateral ligament (ALL). Pop T= Popliteal tendon
Researching for a quick not to mention totally sure resolution to the thesis creating problem? Become dependable crafting company right here. Top notch, instant finishing, well timed interaction best essay.